| As Fauci (who tends to be forthright) confirms, the CDC’s original guidance that Americans did not need to wear masks wasn’t based on the fact that masks made no difference in infection control in daily life. The critical factor in the original decision not to recommend that Americans wear masks was that there weren’t enough masks for healthcare workers fighting COVID-19 on the front lines. Now, the CDC’s guidance has changed, and Americans are urged to wear cloth masks instead, still conserving the most effective masks — medical N95s and surgical masks — for nurses and doctors and first responders.
A Thorny Problem: Mask Supply
Everywhere we turn, we see that the shortage of masks and other PPE, particularly in hospitals, has been acute in the US. A survey of mayors in more than 200 US cities in March found that more than 90% of the cities did not have an adequate supply of masks for their medical personnel and first responders (including police, fire, and EMTs). (“Inside the start of the great virus airlift,” Axios, March 29, 2020, https://www.axios.com/coronavirus-airlift-masks-medical-supplies-1d1913bf-744e-41cf-895c-d8934afa2c36.html)
Doctors and nurses have often had to reuse masks for days or even weeks, laboriously cleaning them as best they can, and falling back on masks hand-sewn by friends and relatives. (“People around the country are sewing masks. And some hospitals, facing dire shortage, welcome them,” CNN, March 24, 2020, https://www.cnn.com/2020/03/24/us/sewing-groups-masks-coronavirus-wellness-trnd/index.html)
Because they lack adequate masks and PPE for effective infection control, US healthcare workers are falling sick and dying. In California, 10% of the infected are healthcare workers. (Becker’s Hospital Review, April 9, 2020, https://www.beckershospitalreview.com/public-health/10-of-covid-19-cases-in-california-are-healthcare-workers-new-york-hospitalizations-trend-down-22-other-updates-from-the-6-hardest-hit-states.html)
China is the world’s biggest producer of medical face masks. It made about half of the world’s $11.7 billion supply in 2018, according to United Nations trade data. And the US has long been China’s biggest customer for masks. But with China facing its own COVID-19 crisis and its factories shuttered, exports of masks plummeted. China imported two billion masks in a five-week period starting in mid-January, a quantity equal to about two and a half months of global production. Anyone who tried to order medical N95s in the second half of January could readily see that the global supply of masks was already being hollowed out by the urgent need in China. In February, the US actually ramped up its exports of masks to China some eight-fold, from the normal $2 million worth to $16 million.
Then, as the virus spread and China brought outbreaks under control, the tables turned; and now China has become a major part of the global masks solution. The country has increased production by nearly 12 times the previous level of 10 million masks a day – a huge mobilization effort.
(“Coronavirus Battle Creates a Global ‘Free-for-All’ to Find Masks,” New York Times, April 1, 2020, https://www.nytimes.com/2020/04/01/business/coronavirus-china-masks.html)
On Sunday morning March 29, a plane from China arrived at John F. Kennedy International Airport, carrying 130,000 N95 masks, 1.7 million surgical masks, 12 million gloves, 50,000 gowns, 130,000 hand sanitizer units, and 36,000 thermometers. It was the first of 22 such flights booked for the following two weeks, according to Rear Adm. John Polowczyk, who runs FEMA’s coronavirus supply chain task force.
At the same time, rather than procuring masks and other critical PPE and coordinating their distribution according to need, the Trump administration was telling the states that they needed to go out and procure their own PPE. Since then, states’ attempts to do so through direct contacts with Chinese companies have been fraught with peril. The incredible demand for masks and other PPE has led to an influx of new companies producing the items, with a resultant falloff in both quality and business ethics. Customers scramble to outbid one another while companies demand full payment up front – and then sometimes disappear with the money.
The Chinese government has responded to this free-for-all by requiring the inspection of every shipment of masks, ventilators, and other medical supplies before export; but that requirement means delayed arrival of critical PPE at hospitals around the world.
(“Coronavirus: inside China’s ‘Wild West’, where ‘mask machines are like cash printers’,” South China Morning Post, April 17, 2020, https://www.scmp.com/economy/china-economy/article/3080378/coronavirus-inside-chinas-wild-west-where-mask-machines-are)
The procurement difficulties faced by states and private entities worsened in many cases after control of the federal COVID-19 response was moved from the Dept. of Health and Human Services to FEMA on March 19. Soon reports began to emerge of FEMA’s requisitioning and redirecting shipments of PPE. In Kentucky, for example, the head of a hospital system told members of Congress that his broker had withdrawn from an agreement to deliver four shipments of much-needed medical supplies after the order was commandeered by FEMA. (“‘Swept Up by FEMA’: Complicated Medical Supply System Sows Confusion,” New York Times, April 6, 2020, https://www.nytimes.com/2020/04/06/us/politics/coronavirus-fema-medical-supplies.html)
Hospitals in search of masks have fared no better. Here is a harrowing first-person account from a chief physician executive of a health system in Massachusetts, detailing his trials and tribulations in securing a shipment of masks – and keeping them out of federal hands: “In Pursuit of PPE,” New England Journal of Medicine, April 17, 2020, https://www.nejm.org/doi/full/10.1056/NEJMc2010025.
Governor J.B. Pritzker of Illinois is among those governors and mayors who have decided to try to outmaneuver the federal government to prevent shipments of masks and other vital supplies from being seized by FEMA for the national stockpile. The Chicago Sun Times reports that he is arranging secret flights out of China to obtain what Illinois needs in the state’s fight against the coronavirus. (“Pritzker arranging secret flights to bring millions of masks and gloves to Illinois,” Chicago Sun Times, April 14, 2020, https://chicago.suntimes.com/coronavirus/2020/4/14/21221459/pritzker-secret-flights-china-illinois-ppe-trump-coronavirus)
The Trump administration has also withheld distribution of PPE from the Strategic National Stockpile. On Thursday April 2, Jared Kushner, who has been given an increased role in the White House’s COVID-19 response, said, “The notion of the federal stockpile was, it’s supposed to be our stockpile. It’s not supposed to be states’ stockpiles that they then use.” (“Trump admin tries to narrow stockpile’s role for states,” AP, April 4, 2020, https://apnews.com/74926f591522b30cbd96853bbcf2dbbd)
It turns out, in any case, that the stockpile’s supply of masks was never replenished after 85 million N95 masks and millions of other protective masks were distributed during the 2009 swine flu pandemic. At the start of the SARS-CoV-2 outbreak, the stockpile held only about 12 million of the 3.5 billion N95 masks that federal officials estimated the healthcare system would need to deal with the pandemic. That shortfall stems from the fact that congressional appropriations for the stockpile are limited; and in the wake of 9/11, the officials who manage the stockpile opted to focus their limited dollars on preparing for terrorist threats and bioterrorism instead.
To make matters worse, in 2018, the stockpile was taken out of the hands of the CDC; and the assistant secretary for preparedness and response in the Health and Human Services Department was put in charge of it. Most experts agree that the CDC was better suited for operational tasks such as organizing and mobilizing a stockpile.
The bigger picture is that our US healthcare system operates with just enough resources, but “just enough” quickly becomes not nearly enough when an event such as a pandemic suddenly strikes. Greg Burel, who was the director of the Strategic National Stockpile from 2007 until January 2020, notes, “Public health is not well funded at the state level, the locality level, or at the federal level in the United States. It is a chronic problem.”
(“Why We’re Running Out of Masks,” The Atlantic, April 10, 2020, https://www.theatlantic.com/health/archive/2020/04/why-were-running-out-of-masks-in-the-coronavirus-crisis/609757/)
At this point, caught unprepared, the US is paying six times the usual price for masks and sometimes from questionable vendors. (“US Pays High Prices for Masks from Unproven Vendors in Coronavirus Fight,” Wall Street Journal, April 18, 2020, https://www.wsj.com/articles/u-s-pays-high-prices-for-masks-from-unproven-vendors-in-coronavirus-fight-11587218400)
Changing Guidance and Mixed Messages
It is not the successful resolution of the mask supply problem that has changed minds about mask use at the WHO and the CDC. The supply problem persists. Guidance changed for other reasons. (“To mask or not to mask: WHO makes U-turn while US, Singapore abandon pandemic advice and tell citizens to start wearing masks,” South China Morning Post, April 4, 2020, https://www.scmp.com/news/hong-kong/health-environment/article/3078437/mask-or-not-mask-who-makes-u-turn-while-us)
For one thing, the world now knows more about SARS-CoV-2, the coronavirus that causes the disease now dubbed COVID-19, than it did in January, February, and March. Infected people may be either presymptomatic for a day or two or, if they are very lucky, asymptomatic, meaning that they will never feel sick at all. Multiple studies have demonstrated that a significant number of infected people, 20% or more, are not symptomatic when they test positive. The Center for Evidence-Based Medicine (CEBM) has compiled a list of 21 reports and their results: “COVID-19: What Proportion Are Asymptomatic,” https://www.cebm.net/covid-19/covid-19-what-proportion-are-asymptomatic/.
An astonishing percentage of the hundreds of sailors who have tested positive aboard the USS Roosevelt, fully 350 of 600, were asymptomatic at the time. (“SECDEF: Majority of Roosevelt sailors with COVID-19 are asymptomatic,” Navy Times, April 16, 2020, https://www.navytimes.com/news/coronavirus/2020/04/16/secdef-majority-of-roosevelt-sailors-with-covid-19-are-asymptomatic-flattop-still-wartime-ready/.)
Furthermore, in another study, close to half of all secondary cases appear to have been infected when the person who infected them had not yet experienced symptoms. (“44% of secondary COVID-19 cases linked to presymptomatic patients,” Becker’s Hospital Review, April 17 2020, https://www.beckershospitalreview.com/public-health/44-of-secondary-covid-19-cases-linked-to-presymptomatic-patients-study-suggests.html)
Infections transmitted by asymptomatic or presymptomatic cases, US health experts realized, posed a gaping hole in the nation’s pandemic containment strategy. Their Asian counterparts, on the other hand, were not surprised. George Gao, director-general of the Chinese Center for Disease Control and Prevention (CDC), expressed concern about Western guidance that suggested only healthcare workers need masks in a Science magazine interview published online on March 27:
“The big mistake in the US and Europe, in my opinion, is that people aren’t wearing masks. This virus is transmitted by droplets and close contact. Droplets play a very important role — you’ve got to wear a mask, because when you speak, there are always droplets coming out of your mouth. Many people have asymptomatic or presymptomatic infections. If they are wearing face masks, it can prevent droplets that carry the virus from escaping and infecting others.” (“Not wearing masks to protect against coronavirus is a ‘big mistake,’ top Chinese scientist says,” Science, March 2020, https://www.sciencemag.org/news/2020/03/not-wearing-masks-protect-against-coronavirus-big-mistake-top-chinese-scientist-says)
People in Asian countries have long worn masks when they are sick to prevent infection, as a courtesy to others and a protection for society, and people there have the 2003 SARS experience with a deadly contagion to remember by. (“Coronavirus: Why some countries wear face masks and others don’t,” BBC, March 31, 2020, https://www.bbc.com/news/world-52015486)
As a case in point, the City of Hong Kong has insisted on masks from the start, but has also implemented vigilant testing, contact tracing, isolating of cases, and social distancing measures. Having done all this, top epidemiologists there still give masks a great deal of the credit for the fact that Hong Kong cases have not spiked:
“‘If not for universal masking once we depart from our home every day, plus hand hygiene, Hong Kong would be like Italy long ago,’ said K.Y. Yuen, a Hong Kong microbiologist advising the government. ‘If you look at where we’ve had clusters, it’s places where the masks come off, like hot-pot family dinners or Buddhist temples.’”
(“Hong Kong Shows the World Masks Work,” Wall Street Journal, April 8, 2020, https://www.wsj.com/articles/to-curb-the-coronavirus-hong-kong-shows-the-world-masks-work-11586338202)
Western countries, on the other hand, are not accustomed to wearing masks to avoid spreading illnesses, and this reality is obvious today as we see how many people, Donald Trump among them, opt not to wear a mask despite the CDC’s about-face. (“’I’m not going to do it’: Trump rejects his own administration’s advice on masks,” https://www.theguardian.com/world/2020/apr/03/im-not-going-to-do-it-trump-refutes-his-own-administrations-advice-on-masks)
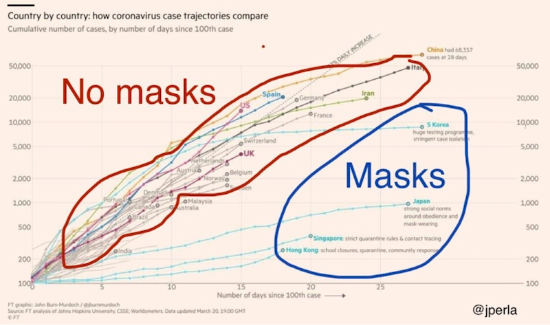
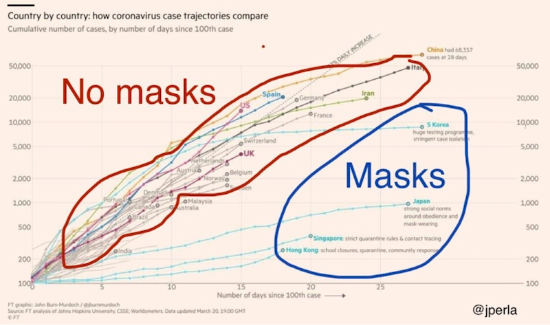
The push for a change in guidance came not only from the evidence but through social media. For example, Jo (@jperla), an autonomous engineer, noted, using a Financial Times graphic updated March 20, outcomes for countries using masks versus countries not using masks. The countries requiring or advising masks for all, however, are also countries that are implementing extensive testing, quarantines, and other measures to control spread of COVID-19.
The chart went viral. |
Leave a Reply
You must be logged in to post a comment.